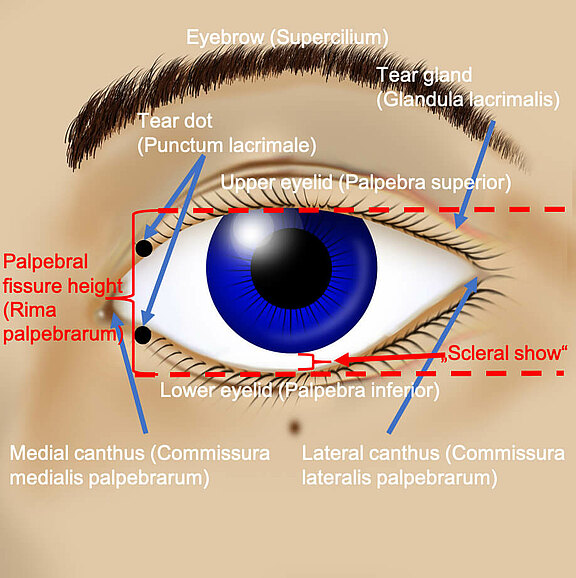
Due to facial paralysis, the facial nerve branches to the orbicularis oculi become non-functional and therefore the muscle around the eye loses its tone (low continuous muscle tension). This loss of tone leads to an increased pulling effect of the "heavy cheek tissue" on the lower lid. This pulls the lower eyelid away from the eyeball. The eyelid is deeper, the palpebra aperture (distance between upper and lower eyelid) widens and the white sclera of the eye below the iris, between the iris and lower eyelid, becomes conspicuously visible. This is called increased "scleral show". In addition, there may be chronic conjunctivitis (inflammation) of the eye, which is manifested by a redness, especially of the eyelids.
If the slackening of the orbicularis muscle and the lower eyelid is pronounced, the wetting of the cornea will complicate several phenomena:
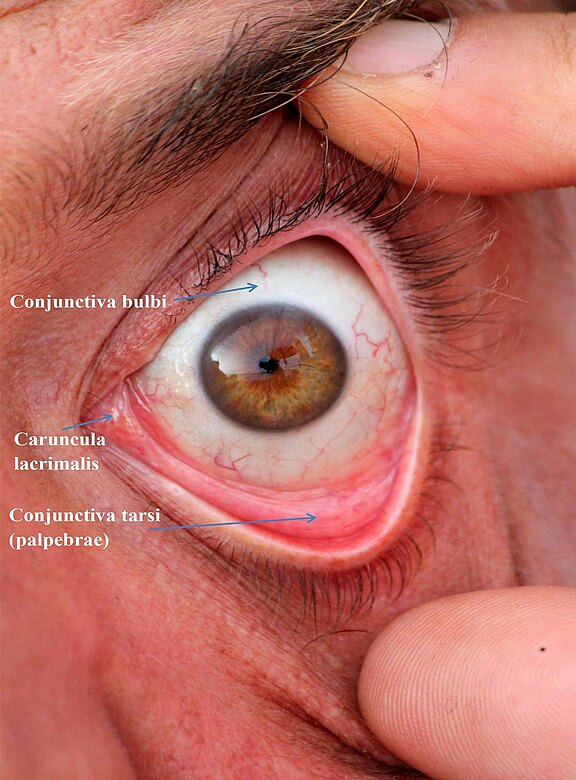
1) The flow of tears produced by the tear gland in the outer upper part of the eye socket and which has a continual physiological wetting of the eye as its task is not directed. Physiologically, it flows over the entire eye and collects at the "tear lake" (Lacus lacrimalis) at the inner eyelid angle. From here the tear fluid is diverted via the lacrimatal puncta (Punctum lacrimale) into the small lacrimal canals (Canaliculi lacrimalis) and via the lacrimal canal system into the nose. If the physiological direction of the tear film is hindered by the flaccidity of the eyelids, the fluid runs from the eye to the cheek via the lower lid, which is sometimes flaccid like a hammock, via the lowest middle part of the eye. This pathologic tearing is called epiphora. Although the eye optically appears to produce too much tear fluid, a "dry eye" appears because there is no uniform tear film for wetting.
2) The slackening of the muscle and a reduced or missing blinking reflex lead to a second phenomenon: the muscle pump function of the orbicularis oculi muscle (eye ring muscle) on the lacrimal canal system is missing. As a result, considerably less tear fluid is "pumped" into the noses, which also has a negative effect on the symptoms of tear flow described in point # 1.
If the sagging of the lower eyelid is still slightly pronounced, a tightening of the lower eyelid with a special suspension technique (canthoplasty, cantopexy), usually at the outer edge of the eyelid, can be achieved. The small operation is performed via an inconspicuous incision in the area of the eyelashes. The scars are not very visible later. Sometimes the inner edge of the eyelid must also be tightened, or the lacrimal puncta must be rotated inwards in order to be able to drain the tear lake adequately again.
If the lower eyelid ectropion is more pronounced, the local tissues are structurally weakened to such an extent that a sole suspension and tightening are not sufficient. Then structurally supporting autologous tissue is introduced, e.g. from the forearm (small parts of a tendon) or the thigh (connective tissue), which are obtained through inconspicuous incisions. Autologous tissue strengthens the sagging tissues on the lower lid through its own structure, which is then apposed to the eyeball again. This allows the eyelid axis to be corrected and returned to its original physiological position. Autologous tissue is hardly perceptible from the outside and fits very well into the anatomy of the lower eyelid.
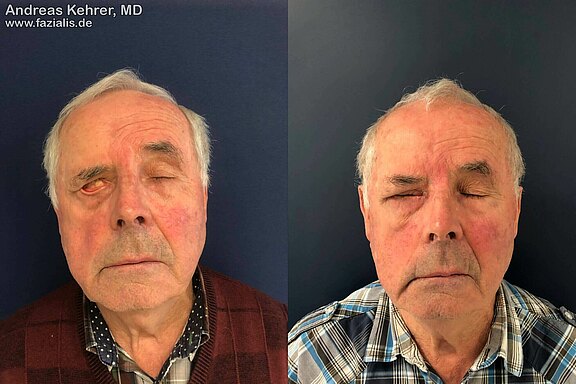
Before the operation, this 80-year-old patient shows a massive tear run over the lower lid edge due to the paralyzed orbicular oculi muscle with dry eye. In particular, it demonstrates a clear malposition of the lower left eyelid (top left picture). Right upper picture: the reconstruction of the lower eyelid with the patient's own tissue shows that the natural flow of tears towards the center of the eye is clearly more directed, the cornea is better wetted, no more pathologic tears are running. Symmetry is improved by raising the eyebrows.
Picture bottom left: A gold implant has already been inserted to weight the upper lid. Due to the flaccidity of the lower eyelid due to muscle weakness, a complete closure of the eye is still not possible. Picture below right: after lower lid reconstruction, an almost complete eye closure is possible. The "irritable conjunctivitis" (conjunctivitis caused by dehydration and constant strain) of the left eye has resolved.
This gentleman suffers from a chronic Bell’s palsy. After more than a year of waiting, the symptoms had hardly subsided. He suffered the most from a pronounced lower lid-ectropion. There was massive lax lower lid tissue and a completely flaccid orbicularis oculi muscle. At the attempt of an eye closure a lagophthalmos (pathological incomplete eye closure) of more than 1 cm remained preoperatively. The insertion of a hidden platinum weight into the upper eyelid and a very thin strip of tendon from the forefoot into the lower eyelid resulted in a complete closure of the eye again. The cornea, which is important for the visual sense, is protected again and the patient will also no longer suffer from conjunctivitis. A further surgical step will include a right brow lift in order to further improve the resting facial symmetry.