The eye complex can be significantly affected by facial paralysis. Limited function of eye muscles may be one sign facial palsy. It is interesting to note that children and adolescents are functionally and aesthetically less affected in this area of the face, even in case of complete facial paresis.
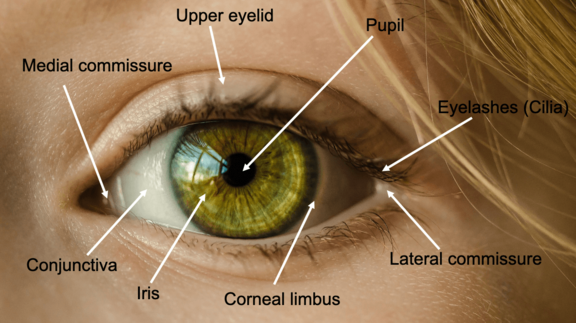
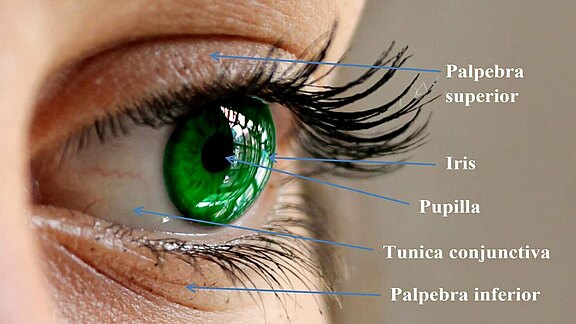
Eyelid closure is mediated by the mimic muscles, especially the orbicularis oculi muscle. It plays an important role in the moistening of the cornea and prevents its dehydration by regular wetting with tear fluid.
Lagophthalmos is a symptom representing incomplete closure of the eyelids of one or, more rarely, both eyes. The reasons for this can be manifold, the cause can be congenital malformations, traumatic damage and very often a nerve paralysis ( fascial paresis). Paresis can be congenital or acquired.
What happens when affected patients can no longer close their eyelids completely?
The surface of the eye (cornea) is normally moistened, protected and disinfected by a regular tear film. If this tear film is inadequately distributed due to insufficient eyelid closure, severe clinical pictures with accompanying visual deterioration, visual impairment or destruction of the cornea can result, leading to complete loss of visual acuity. These consequences can sometimes occur within a few days or weeks.
In order to avert serious consequential damage, the cornea must be protected at all costs. Various conservative and surgical methods are available.
Since the facial nerve a significant role in the production of tears, the manufacturing of tear fluid may be reduced, thus further increasing dryness of the eye. If the lower eyelid is very flaccid, there is "sagging" in the middle of the lower eyelid. This is referred to as lower eyelid ectropion. In extreme cases, the eyelid and eyeball lose contact. The continuous flow of tears, which, physiologically speaking, is regulated in the outer upper lid - where the tear gland is located- via the convex eyeball to the middle of the eye, is impaired. Tear fluid collects in the area of the lower eyelid forming a "lake of tears", which in turn impedes the free vision of the pupil, and thus sharp vision, in some patients. Frequently, the fluid runs over the edge of the lower eyelid onto the cheek and chronic watering (epiphora) develops. A reduced or even completely deactivated pumping function of the eye ring muscle in the area of the lacrimal canal system in the inner corner of the eye, which begins at the tear spots visible at the edge of the lower eyelid, also intensifies the condition. Ironically, the patient still has to struggle with a dry eye because the tear fluid is not evenly distributed. A slowed or absent blinking reflex also plays a role in facial paresis.
This three-dimensional model shows, among other things, the corneoscleral trabecular meshwork (Trabeculum corneosclerale), which consists of flat connective tissue with pores (Fenestrations). The Trabeculum corneosclerale is involved in the flow control of the aqueous humor and may be involved in subtypes of glaucoma. Furthermore, the course of the aqueous humor can be traced. Formed by the ciliary processes (Procc. ciliares), the aqueous humor passes through the pupil into the anterior chamber of the eye, then flows along the cornea and mostly through the chamber angle (Angulus iridocornealis) into the Schlemm's canal and finally into a venous plexus (Plexus venosus sclerae). It is important to emphasize that the function of the M. orbicularis oris and thus of the N. facialis is essential for the external wetting of the cornea.
Source: Intervoke. Aqueous Humor: The Eyes Trabecular Meshwork 2.0. 2016. sketchfab.com/3d-models/aqueous-humor-the-eyes-trabecular-meshwork-20-0db7a0cc49ea4a31ac3a7ed94909d6e5. Accessed on 11/15/2020. CC BY-SA 4.0. creativecommons.org/licenses/by-sa/4.0.
The reduction in strength or complete malfunction of the upper part of the eye ring muscle can lead to incomplete closure of the eyelid. If the affected person tries to close both eyes slightly, the eye on the affected side cannot be completely closed and the cornea of the eye cannot be adequately protected. Simultaneous sagging of the lower eyelid exacerbates the incomplete closure of the eyelid and expands the cleft eyelid pathologically even further. The result is a greater exposure of the eyeball during eye closure (e.g. during sleep). A chronic irritating conjunctivitis occurs, epitomized by redness and itching. Without medical intervention, "dry eye syndrome" (keratoconjunctivitis) can develop in the further course of the disease. The conjunctiva, but especially the cornea, can suffer permanent damage due to the lack of moistening with tear fluid, which can lead to blindness. To prevent this, there are both conservative and surgical measures (e.g. platinum implant upper eyelid, lower eyelid lift).
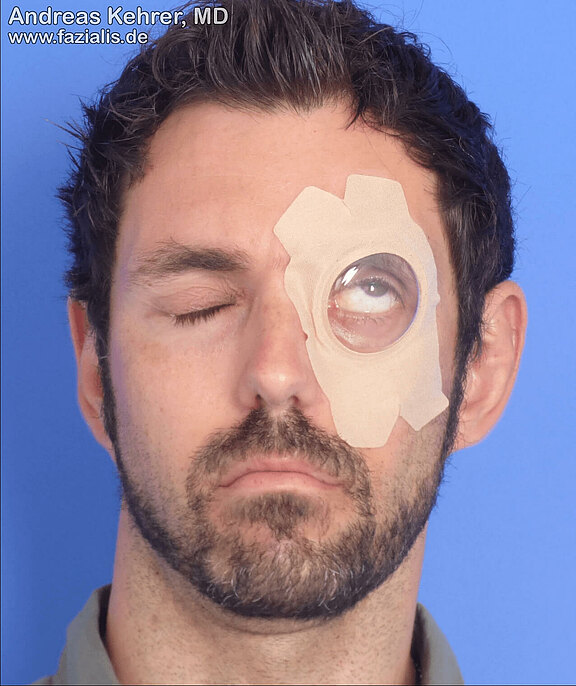
Figure 4
This patient suffered complete facial paralysis due to a skull base fracture. Unfortunately, appropriate measures for eye protection (including surgery, such as platinum weight) were omitted in the initial phase. This resulted in severe conjunctivitis, leading to destruction of the cornea (keratopathy). Unfortunately, the patient can only see black and white on the left side. A corneal transplant would be the only way to regain better vision.
If the corneal erosions are still small, they are sometimes not visible to the bare eye. In this patient, however, they are already visible without magnification. The patient was fitted with a platinum weight to improve eyelid closure. Improved eyelid closure may still result in healing of the erosions.
Physiologically speaking, normal closure of the eyes leads to so-called "Bell’s phenomenon". The eyelid closure reflex causes the eyeballs to roll upwards when the eyelids are closed. The facial nerve is mainly involved in this reflex movement. Since the eyelids normally cover the eye when closing, Bell’s phenomenon is not visible. If, however, facial nerve paresis causes incomplete eyelid closure, the upward movement of the eyeball on the affected side can be observed: white of the eye(sclera) is evident. Bell’s phenomenon is therefore primarily the visible upward movement of the eyeball. It has pathological significance simply because it is only visible when eyelid closure is incomplete.
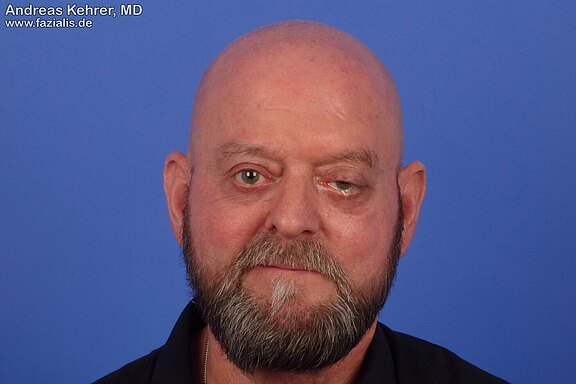
The facial nerve is also, at least partially, responsible for the (involuntary) blink reflex. If the corresponding nerve branch (partially) fails, the blink reflex is also significantly reduced. In this 71-year-old patient, this can be clearly observed in the right eye: there is considerably less moistening of the cornea with tear fluid. Consequently, the patient complains of a very dry eye. The flow of tears towards the middle of the eye is additionally impeded by a sagging lower eyelid. The loss of the forehead branch results in paralysis of the forehead muscle, so the eyebrow is about 2 cm lower at rest than on the opposite side.
The loss or weakness of the eye ring muscle often leads to a distinct slackening of the lower eyelid. Since the lower eyelid is now structurally weakened by reduced muscular function, the remaining eyelid structures are dilated. The fine cartilage plate of the lid edge is also affected, so that the lower lid sags. A so-called ectropion has developed. This can have its maximum medial (towards the centre of the body) or lateral (away from the center of the body), but in most cases the largest dilatation occurs centrally. In this patient, the result is an undirected flow of tears which no longer finds its way completely to the inner corner of the eye. A watering eye occurs because the tears spill over the edge of the eyelid. Paradoxically, patients often complain about ‘’dry eye’’ ("itchy conjunctivitis"), although the eye appears too moist to the observer. A lower eyelid lift, which can often be achieved laterally by shortening the tarsal cartilage, is a remedy. It is often combined with a medial tightening. If the ectropion is very pronounced, the lower eyelid must be structurally supported in order to reconstruct the ectropion, i.e. a small tendon strip (e.g. from the forearm or forefoot) must be inserted to reinforce it. This is externally very inconspicuous.