Pathophysiology (ancient Greek páthos "disease" and physiology explained in the previous section) is the study of the description of pathological processes or changes in physiological processes in the body.
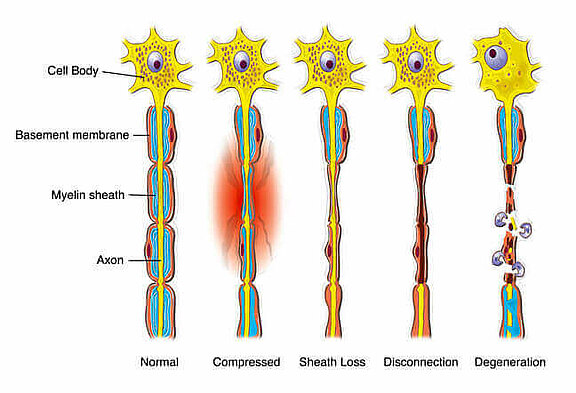
Peripheral facial paresis can have numerous causes, which are explained under the tab "Facial Paralysis - Causes". Basically, damage to a peripheral nerve follows the principle of "Wallerian degeneration" [1]. Possible are traumatic severance (axonotmesis), bleeding, deficiency, bruising, infections or toxic damage.
Source: Pubslished as “Terri”, Medatrio, Degeneration & regeneration of peripheral nerves, n.d., medatrio.com/degeneration-regeneration-of-peripheral-nerves, accessed on 08/28/2020.
The degeneration proceeds as shown in the schematic drawing (fig. 1) and is initially characterized by damage to the myelin sheath, which isolates the nerve from the environment like a rubber sheath on a power cable. The Schwann cells (insulation cells of the myelin sheath) are eliminated by macrophages (endogenous cells specialized in the degradation of cells) as part of an inflammatory reaction. If the nerve is now exposed without a protective sheath (like the fine copper wires of a power cable lying in the water), the impulses can no longer be transmitted correctly at this point. This loss of function and stress caused by the inflammatory reaction now also cause the axon to degenerate. The open axons are now also degraded by the macrophages (eating cells of the immune system), which irreversibly destroys impulse transmission [1].
Proximal (towards the cell body in the brain) the nerve "lives" on, while the distal part dies and loses its function. However, it remains intact as a structure and can serve as a guide rail for axons sprouting from the living nerve part, provided they can reach it. This is possible if the sheath structure (the myelin sheath) is still intact or if the severed nerve is adapted again by a microsurgical nerve repair.
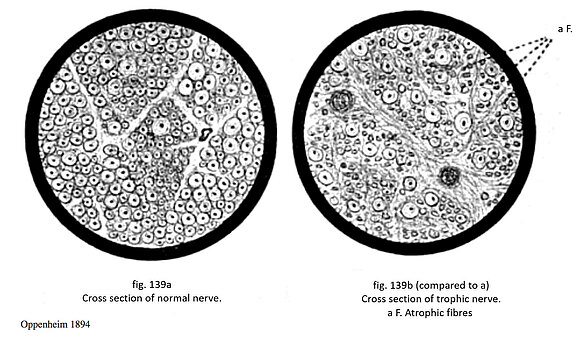
In 1894, Oppenheim investigated cross-sections of healthy and damaged nerves and described the differences in nerve fiber qualities. The cross-sectional drawing (fig. 2) of a peripheral nerve shows normal, healthy axons with different physiological degrees of myelinization. The right picture shows the cross-section of a damaged nerve. A significantly reduced density and number of axons (nerve fibers) is shown. A large number of nerve fibers are "atrophied", i.e. have undergone an irreversible regression to nerve fiber tissue that no longer functions.
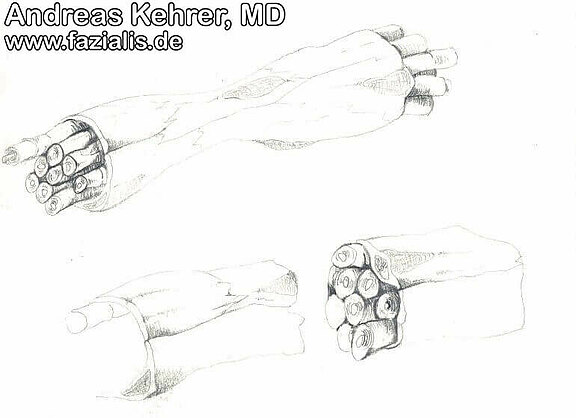
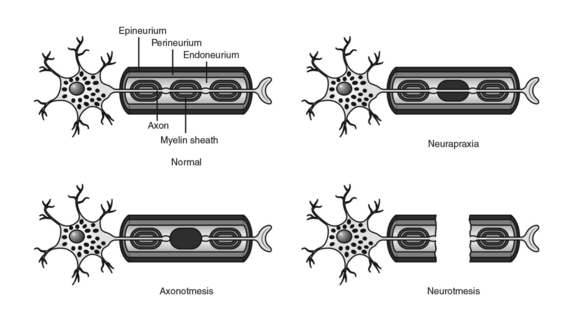
Such damage (fig. 3) can either cause a temporary loss of function (neuropraxia) with loss of all or part of the fascicles/axons, or a long-term permanent damage (axonotmesis, e.g. 4-6 months) until irreversible loss of function due to massive scarring. The lower picture shows a complete separation of the nerve with its envelope structures (neurotmesis). The axons on the left (far from the brain) have already lost their sheath layer (demyelination), on the right (near the brain) they are still alive. If continuity (e.g. nerve repair) is restored promptly, the axons can sprout in from the right and make the nerve functional again. Otherwise, the nerve is irreversibly damaged and the controlled facial muscles perish (fatty degeneration).
These nerve fibers are no longer available for nerve excitation and muscle activation. Concurrently, there is a comparatively large amount of connective tissue, which additionally inhibits the transmission of excitation by the nerve. The result is far less "current flow" to address a facial muscle. If the "current flow" is so low that a minimum excitation threshold of the facial muscle is no longer reached, not only is the muscle weakened, but complete paralysis occurs.
If facial paresis also involves nerve fibers of the neighboring nerves (intermediate nerve or the superficial nerve), tear secretion is reduced. In the worst case, the production of tears on the affected side can be completely stopped. Saliva secretion may be reduced if the chorda tympani is involved.
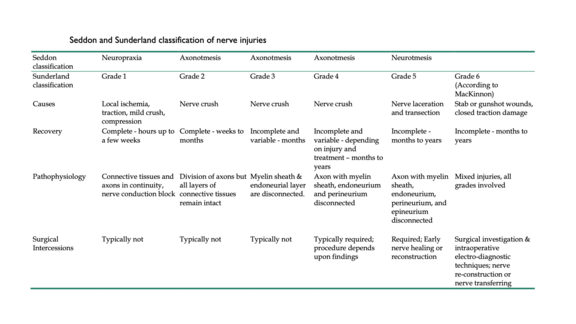
When it comes to the classification of damage to a nerve, the classifications according to Seddon and the Sunderland should be mentioned. Both describe different degrees of nerve lesion called neurapraxia, axonotmesis and neurotmesis (fig. 4).
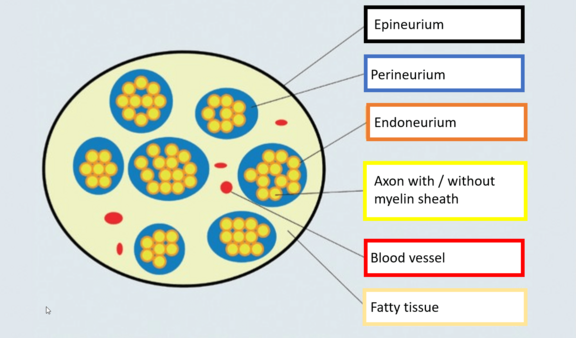
For a better understanding of nerve lesions, the differentiation of the envelope structures of a nerve is essential (fig. 5, fig. 6). Epi-, peri- and endoneurium are found from the outside to the inside. The epineurium embeds the entire nerve in the surrounding structures and consists of reinforced connective tissue.[1] The perineurium combines several nerve fibers, i.e. the unit of nerve cell extension (axon), envelope cells (Schwann cells) and the outermost layer of Schwann cells (neurolemma), to form nerve fascicles. The individual nerve fibres are finally encased by the endoneurium.
Source: Swivel Circle, P. Traumatic peripheral nerve injuries. 2015;DNP 16:43–50. doi.org/10.1007/s15202-015-0839-9.
The continuity obtained is defining for the stage of neurapraxia (Sunderland I)[2] Here, focal demyelination occurs, i.e. a heart-shaped damage of the isolation layer (myelin sheath) of the axon. In this stage, conservative therapy is normally indicated, as spontaneous regeneration usually occurs within days or weeks, thus restoring the desired state (restitutio ad integrum). Causes are, for example, compression or stretching of at least 16%[3] of the affected nerve section, which can result in a deficient blood supply (ischemia).
The stage of axonotmesis (Sunderland II) is characterized by an interruption of the continuity of the axons while the envelope structures are preserved[4] Figuratively speaking: Externally, the nerve may appear intact, but its internal structure may have defects. In addition, the phenomenon of Waller's degeneration becomes apparent. This results in a regression of the damaged nerve cell processes distal to the lesion site.[5]This regression is followed by the growth of new axons at a rate of approximately 1 mm/day.[6] Healing is only possible after months.
A combined lesion of axon and envelope structure is called neurotmesis.[7] Neurotmesis can be further differentiated according to Sunderland. For example, damage to the nerve cell process and endoneurium are characteristics of grade III according to Sunderland. Grade IV includes an interruption of continuity also of the perineurium. If there is a defect in all three envelope structures as well as the axon, the requirements for grade V are met. Grade III is accompanied by bleeding into the endoneurium. Accordingly, the surgical removal of the bleeding (hematoma resection) and the microsurgical removal of constrictions that exert pressure on the nerve (neurolysis of the nerve) are useful therapeutic options. In contrast to grade IV and V, grade III allows (partial) healing after months. In this respect, a proactive approach in the form of a tension-free fascicle suture or neurolysis is indicated for grades IV and V.[8]
According to Millesi, third-degree lesions can be described more precisely.[9] Grade III A is accompanied by pathological proliferation of the connective tissue (fibrosis) of the epifascicular epineurium located on the surface of the fascicles. In grade III B fibrosis is found in the interfascicular epineurium, i.e. between the fascicles. Grade III C is defined by fibrosis of the endoneurium.
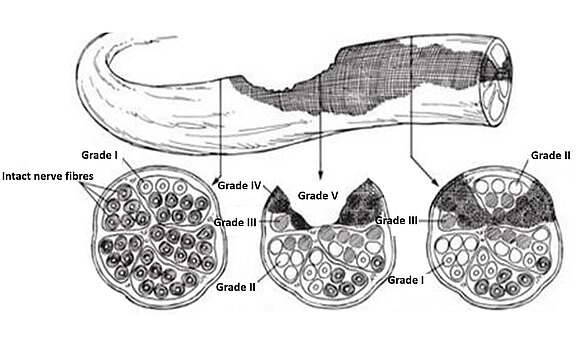
It should be emphasized in particular that neurapraxia, axonotmesis and neurotmesis can be present simultaneously[9] Thus, a nerve cross section or longitudinal section can simultaneously show intact areas and sectors with different lesion characteristics (fig. 7).
This seems to occur comparatively frequently in the section of the facial nerve during its course in the narrow petrous bone canal (Canalis n. facialis) and can explain the inconsistent patterns of different muscle groups in the face as well as their temporal course with healing taking place or failing to heal.
Figure 7
The upper part of the image shows a nerve section in longitudinal section. The arrows mark individual sectors in the nerve course. These sectors are shown in cross section in the lower image section. It becomes clear that damage to a nerve section can manifest itself in different ways in both longitudinal and cross-sectional views.
A peripheral nerve, such as the facial nerve, is a bundle of numerous nerve fibers together with their sheath layers. For example, in the case of a nerve squeeze, it is possible that some fibers merely cut through the axon while preserving the connective tissue sheath, while other nerve fiber bundles are completely severed. Accordingly, different degrees of nerve damage can occur in a nerve and consequently different Sunderland stages (fig. 7). This complete or partial nerve damage, for example through constriction in the facial canalis in the petrous bone, manifests itself in facial nerve palsy in the form of complete or incomplete facial paralysis, i.e. paralysis of the mimic muscles (see chapter "Facial Paralysis").
If nerve fibers of the adjacent nerves in the temporal bone (intermediate nerve or the petrosus superficialis major nerve) are involved in facial nerve palsy, tear secretion may also be reduced. In the worst case, tear production on the affected side can be completely absent. Salivary secretion and taste sensation are reduced if the Chorda tympani, another branch of the facial nerve, is involved. The following 3D model shows the course of the facial nerve and the constriction in the petrous bone.
If damage to the facial nerve occurs, for example due to pressure damage caused by swelling (viral infection, Bell’s palsy) in the temporal bone, the nerve fibers are separated at the site of damage, comparable to many individual veins of a thick electrical cable (fig. 8). As an example, the yellow fibers have the task of targeting the muscles of the eye complex, the blue fibers the muscles of the corner of the mouth region.
If the nerve healing process now leads to an incorrect connection, i.e. some yellow fibers incorrectly combine with blue fibers, the muscles of the eye complex, such as the ring muscle, are also unintentionally moved when the muscles of the mouth region are actuated, since the impulse at the damage site of the nerve is also transmitted by the wrong fibers. An unintentional mass movement ("synkinesis") has developed. If the patient now smiles with incomplete facial paralysis, the eye closes at the same time. If the nerve fibers are overexcited, spastic cramps can also occur, which are often visible in the eye (blepharospasm).
Source: Luhansk Telegraph, Republican Truth, Broken cable caused disruptions in the work of Internet providers in the Republic - the Ministry of Communications of the LPR, Luhansk, 10/18/2016, lgt.su/lnr/respublika/8890-razryv-kabelya-stal-prichinoy-sboev-v-rabote-internet-provayderov-v-respublike-minsvyazi-lnr.html, accessed on 08/28/2020.
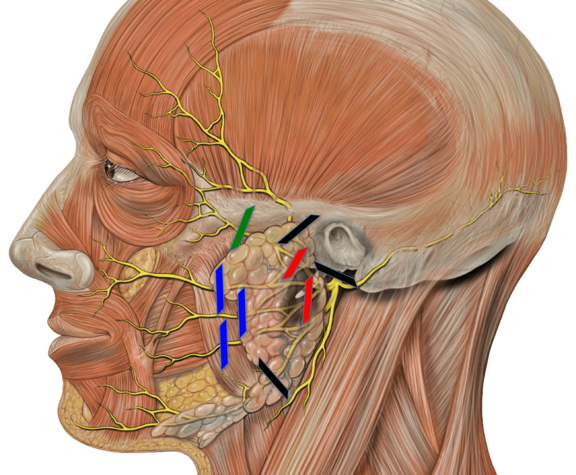
Only one branch can be affected, which can lead to isolated failure symptoms (fig. 9). The diagram shows schematically possible lesion locations (colored lines) from which the expected loss of function can be derived. For example, with the green lesion line, failures in the area of the eye-ring muscle are to be expected. In the "anatomy" section, the variability of the nerval innervation and especially the cross-linking under the branches has already been described. Therefore, the individual functional failures of affected patients can be very diverse.
Source: Modified by author: Patrick J. Lynch, Dr. C. Carl Jaffe, Head facial nerve superfical branches, 12/23/2006, commons.wikimedia.org/wiki/File:Head_facial_nerve_branches.jpg, accessed on 08/28/2020, CC BY-SA 2.5. creativecommons.org/licenses/by-sa/2.5.
Sources:
[01] Normale Anatomie und Histologie des peripheren Nervens. In: Müller-Vahl H, Hrsg. et al. Läsionen peripherer Nerven und radikuläre Syndrome. Thieme. Stuttgart. 2014 10th ed. P6. doi: 10.1055/b-0034-97215.
[02] Einteilung traumatischer Nervenläsionen. In: Müller-Vahl H, Hrsg. et al. Läsionen peripherer Nerven und radikuläre Syndrome. Thieme. Stuttgart. 2014 10th ed. P41. doi: 10.1055/b-0034-97215.
[03] Wanschitz J. Pathophysiologie von Nervenläsionen. Neurologisch 2013; 2:1–3.
[04] Seddigh S. Traumatische Nervenläsionen. Trauma Berufskrankh 19 2017; P340–346.
[05] Coleman MP, Freeman MR. Wallerian degeneration, wld(s), and nmnat. Annu Rev Neurosci. 2010;33:245-67. doi: 10.1146/annurev-neuro-060909-153248. PMID: 20345246; PMCID: PMC5223592.
[06] Senger D, Erbguth F. Critical-illness-Myopathie und -Polyneuropathie [Critical illness myopathy and polyneuropathy]. Med Klin Intensivmed Notfmed. 2017 Oct;112(7):589-596. German. doi: 10.1007/s00063-017-0339-0. Epub 2017 Sep 5. PMID: 28875277; PMCID: PMC7095927.
[07] Kaya Y, Sarikcioglu L. Sir Herbert Seddon (1903-1977) and his classification scheme for peripheral nerve injury. Childs Nerv Syst. 2015 Feb;31(2):177-80.
[08] Pereira T, Gärtner A, Amorim I, Almeida A, Caseiro AR, Armada-da-Silva PA, Amado S, Fregnan F, Varejão AS, Santos JD, Bartolo PJ, Geuna S, Luís AL, Mauricio AC. Promoting nerve regeneration in a neurotmesis rat model using poly(DL-lactide-ε-caprolactone) membranes and mesenchymal stem cells from the Wharton's jelly: in vitro and in vivo analysis. Biomed Res Int. 2014;2014:302659. doi: 10.1155/2014/302659. Epub 2014 Jul 10. PMID: 25121094; PMCID: PMC4119891.
[09] Einteilung traumatischer Nervenläsionen. In: Müller-Vahl H, Hrsg. et al. Läsionen peripherer Nerven und radikuläre Syndrome. Thieme. Stuttgart. 2014 10th ed. P41. doi: 10.1055/b-0034-97215.