For years we have specialised in the therapy of early (acute) and chronic facial paralysis. Surgery for facial paralysis always has functional and aesthetic aspects. A facelift alone certainly does not do justice to the complex clinical picture. Our team offers the entire internationally proven surgical spectrum, holistic treatment and any recognized non-surgical treatments and microsurgical reconstruction options for facial paralysis. Thanks to regular exchange with international specialist centres, continuous further training for specialisation and ongoing research projects, treatment concepts and surgical procedures can be offered that correspond to the highest and most up-to-date scientific standards as well as international standards. The therapy is always adapted to the patient as an individual and determined together with the patient. Individual, tailor-made solutions for patients often offer the greatest success. In principle, there are no restrictions with regard to age or existing concomitant diseases. Some surgical methods can be performed under local anesthesia (local anesthesia), other more profound corrections are offered under gentle general anesthesia. In the case of asymmetries of patients with incomplete facial paralysis (partial paralysis of one half of the face), injection treatments (e.g. with botulinum toxin, "Botox" or autologous fat, termed lipofilling or lipografting) may be used and surgery may not be necessary at all.
Enclosed we would like to point out once again the importance of early therapy. People affected by partial or complete facial paralysis often have to struggle with very severe functional and aesthetic limitations. Often their suffering robs them of a lot of self-esteem and social interaction. However, in contrast to the past, patients today, especially in the case of irreversible loss of function of the facial nerve, no longer have to accept their fate in the same way. Even if the facial nerve no longer functions: there is much hope for significant improvement. Unfortunately, the following situation has become apparent in many countries: on the one hand, there are very many affected persons (about 20-30/100,000 people, about a quarter of whom suffer permanent functional loss) who are not sufficiently helped, and on the other hand, there are very few solid points of contact for an adequate operative restoration of function, facial expression, symmetry and form.
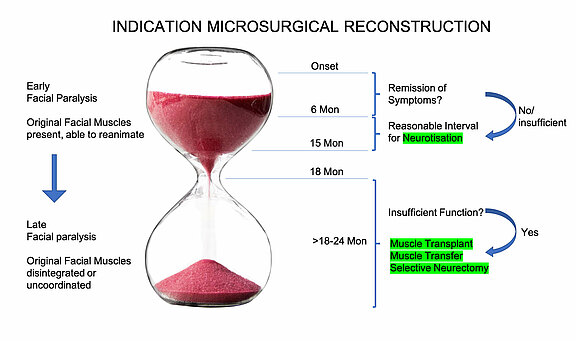
The reality of facial patients is often somewhat frightening. Patients are often put off for a very long time (more than 1-1.5 years) with futile waiting for an (often unrealistic) improvement, while the mimic musculature is constantly diminishing and finally lost due to the lack of nerve stimulation despite consistent physio-/ergotherapy and speech therapy. Atrophy of facial muscles occurs: a continuous, irreversible transformation into fatty tissue, which is irreversibly completed after about one and a half to two years. Even then, a free muscle transplantation or muscle rearrangement (temporalis transfer) can still help well. Using modern microsurgical methods as free functional muscle transplantation (e.g. of a small gracilis muscle from the thigh) are then also very successful and may produce well-functioning and reproducible results in our hands. However, although they are able to alleviate much of the patient's suffering, it is obvious that a single transplanted muscle can only replace part of the function of 21-24 facial muscles of one half of the face with different vectors. In the early-secondary stage, i.e. after waiting for a primary phase of about 6 months (max. 9-12 months), a gentle nerve rearrangement ('nerve transfer') of a lower branch of the masticatory nerve, possibly with an additional nerve transplantation (from 6 months after the onset of paralysis without signs of improvement) is therefore much more elegant and easier to perform in order to maintain or regain important functions. In the best case all 21-24 facial muscles can be preserved. Nerve relocation ('nerve transfer') and transplantation do not have any significant functional disadvantages for the patient. The chewing function is completely preserved.
It would therefore be very helpful for this part of the patient if a more timely indication for nerve transfer was initiated. The ignorance of these possibilites in micorsurgery and other specialized plastic surgery methods may concern medical colleagues of all disciplines, therapists and of course primarily patients. All too often, it leads to valuable time being wasted unnecessarily in order to preserve the mimic musculature.
In the latest version of the S2-guideline of the German Society of Neurology (DGN) "Therapy of idopathic facial paralysis (Bell's Palsy)" of Februrary 2022, at least the appendix contains recommendations for a much earlier need for surgical action than was practiced in the past in order to preserve potentially functioning facial musculature for the recovery of important functions and facial expression.
Algorithm based on the latest scientific findings for the indication of microsurgical reconstruction procedures. If failure of nerve healing may be expected, neurotisation is in many cases superior to other therapeutic procedures. However, the indication must be established in time to achieve the best functional results.
The long-term prognosis after surgical reconstruction is very good. Regained functions are usually of lasting value. Excluded from this, however, is an increasing laxity of the facial skin with increasing age of the patient. E.g. oral continence once achieved along with a tighting of cheek tissue by static suspension procedure may deteriorate by natural tissue aging again over the course of many years. However, these minor problems are then again accessible for further static reconstruction or tissue tightening. Shifted muscle groups or freely transplanted, functioning muscles, on the other hand, once they have taken up their function, retain it permanently. The same applies to nerve rearrangements and nerve transplants.
Source:
[1] S2-Leitlinie "Therapie der idopathischen Gesichtlähmung (Bell's Palsy)" der Deutschen Gesellschaft für Neurologie (DGN) März 2017: www.awmf.org/leitlinien/detail/ll/030-013.html