Free functional muscle transplants, which today can be performed without a reduction in the function of the donor site, are suitable for patients from 5 years to 75 years old. Free muscle transplants have successfully established themselves according to international standards for "reanimation" of the affected paralyzed half of the face and promise the best results in chronic paralysis after complete loss of the mimetic musculature. This procedure is only offered at specialized facial reconstruction centers that are capable of the entire spectrum of restoration, including microsurgical transplantation. In the case of chronic, i.e. prolonged, facial paralysis, this procedure represents gold standard for reconstruction according to international scientific criteria.
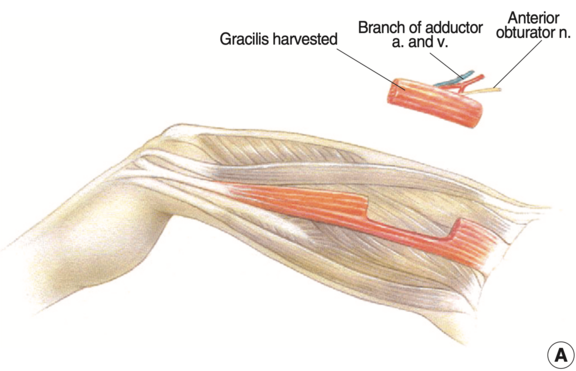
Various muscles are available as donors in the human body for this surgical procedure. When selecting the donor muscle, several factors must be considered including functional deficits after harvest, surgical accessibility, size, strength, and functional design of the muscle must be taken into account. The gracilis muscle has proven itself worldwide as one of the ideal thigh muscle donors for functional muscle transfers. The removal is accompanied by almost no loss of function, as there are several other muscles that can readily assume its function. Excellent results can be achieved with this muscle graft.
We transplanted a small free gracilis muscle from the thigh to this young patient with congenital facial paralysis. The muscle is barely perceptible under the cheek skin. Through muscle muscle transplantation, the smile in the left half of the face (right in the picture) could be harmoniously restored. This function which was completely missing before.
Another option is the pectoralis minor muscle. The surgical approach is more complex than the aforementioned thigh muscle. Nevertheless, this muscle has also proven itself as a functionally high-quality muscle flap and, with its spring-like fibres, has a somewhat more natural vector for controlling the lifting of the corner of the mouth in the face. If there is already a pronounced volume deficit in the half of the face, for example after a tumor resection, which requires balance, we transplant the latissimus dorsi muscle (large, broad back muscle) or a suitable small part of it.
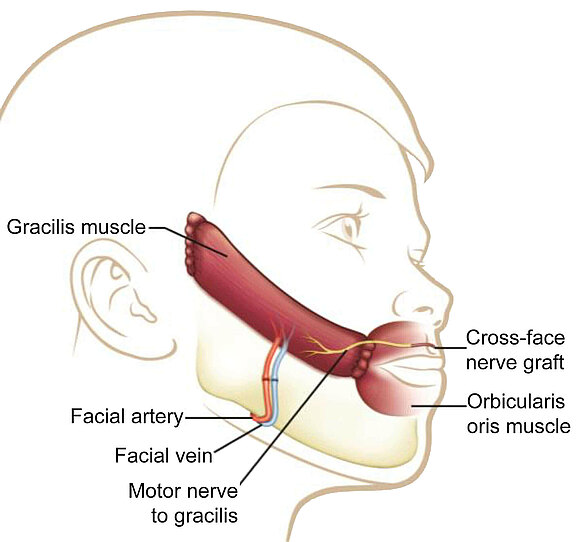
The gracilis donor muscle is gained through a small incision on the inner side of the thigh near the trunk and is transplanted under the cheek tissue through a modified face-lift incision (inconspicuous incision in front of the ear). The microsurgeon uses a surgical microscope to connect it to small vessels for immediate restoration of blood circulation and to a donor nerve in the face. It can be connected by coaptation (microsurgical nerve suture) to previously transplanted donor nerves (cross-face nerve grafts, CFNG), facial nerve branches, or other donor nerves. With the appropriate expertise, the muscle can be shaped to such an extent that it only requires a small amount of effort and is no longer visible under the skin after an initial phase of facial swelling after the operation.
After transplantation, a few months elapse before the muscle is able to take up its activity. In the post-operative "reinnervation phase" (phase of nerve healing) that follows, axons (nerve fibers) must first sprout into the muscle transplant in order to control it.
The Musculus gracilis ("slender muscle") is a skeletal muscle of the thigh close to the surface and is counted among its adductors. Its function can be completely waived, so that no functional deficit arises after harvest. In the following 3D model it is clearly visible on the inner side of the thigh - can you make it out?
Source: Gaia Tech, Bangor, Wales. sketchfab.com/3d-models/leg-with-muscles-cc3585e0154a4060bebfb414dbcd7514
This 45-year-old patient presented with a complete flaccid facial paralysis that had been present for 5 years at the time of surgery (situation left video). He underwent surgery with a free gracilis muscle graft, regeneration of the nasolabial fold, and additional connective tissue from the thigh. Especially complicated is the reconstruction of a strong upper lip lift as well as restoring a, in the course of this, natural smile. Postoperatively, a harmonious symmetrical smile is achieved.
Patients with "only" incomplete paralysis, especially those who have already become accustomed to limited facial expression from birth, are much more difficult to satisfy than patients with marked flaccid paresis. Nevertheless, free muscle grafting to improve symmetry and function may be worthwhile. This patient underwent transplantation of a small gracilis muscle from the thigh to improve smile and mouth angle control. Postoperatively, more maxillary teeth are seen in wide laughter as well as a much more harmonious nasolabial fold (smile line between the nostril and corner of the mouth).
This 37-year-old showed loss of mouth angle control and smile after Bell's palsy. No signs of recovery of the facial nerve were note over a course of 20 months. He was then first transplanted a cross-face nerve graft (CFNG) 20 months after the onset of facial palsy (FP). In a second surgery 32 months after onset of fp a free gracilis muscle was transplanted. This restored a natural smile and laugh and significantly strengthened social function.
Same patient. The upper teeth show is demonstrated very well postoperatively. While before the muscle transplantation no upper teeth were exposed, even in the case of a broad smile trying to show upper jaw teeth, now four teeth flash postoperatively. The smile appears much more symmetrical and from then on the patient consciously uses it again much more often in non-verbal communication.