Selective Neurectomy / Selective Neurolyis
This minimally invasive surgical therapy is mostly considered for patients with synkinesis, spastic muscle groups or hyperactivity of muscles on the non-paralyzed side. In combination with a V-to-VII nerve transfer, this procedure seems to be particularly suitable for synkinesis in smiling.[1] In neurectomy or selective neurolysis, small sub-nerve branches of the facial nerve are specifically switched off while others are spared (see Fig. 1). The expected success of selective nerve elimination is tested in advance with an injection of botulinum toxin. In contrast to "chemodenervation", the drug-based elimination of excessive nerve irritation, surgical neurectomy basically guarantees a permanent result. However, especially nerve fibers that have been severed during the therapy of (periocular) synkinesis around the eye seem to have a high regeneration potential.[2] Overall, selective neurectomy may also improve the alignment and depth of the nasolabial fold.[3]Furthermore, postoperatively more natural movements of the lower lip and oral commissure were observed. Selective neurectomy can be performed through hidden incisions, e.g. through the oral cavity (enoral), under general anesthesia and usually leaves no visible scars. One promising approach is "Symmetrical Facial Repositioning".[4] Depending on the severity of the facial paralysis, this involves removal (resection) of the buccal fat corpuscles, a face lift (rhythidectomy) and a fat graft. This method is combined with selective neurectomy.
This 22-year-old female patient suffered from synkinesis, a typical sequelae of a defect healing of the facial nerve after facial nerve palsy. When smiling, involuntary spasms of unintended muscle groups in the right side of the face occur. The corner of the mouth appears fixed by counterproductive muscle activity, the chin muscle tenses, and the eye involuntarily closes almost completely. In some patients, this can impair vision in everyday life (for example, when driving a car). After surgery by modified selective neurectomy, the face appears much more balanced and relaxed. The corner of the mouth has gained more freedom when smiling, the cramping around the chin and the involuntary closure of the eyes have improved.
This 34 year-old patient complained of the same phenomena. Before the operation, only 1 1/2 maxillary teeth are exposed when smiling broadly on the right side, the corner of the mouth also tends to point downward when smiling ("negative vector") and an unwanted partial eye closure may be noticed. Immediately after selective neurectomy and myectomy, the first improvements can be seen: now 3 maxillary teeth are exposed when smiling, the corner of the mouth has a "positive vector" (points upwards) and the eye is clearly more relaxed. In order to reorganize the mimic function, intensive professional as well as additional independently performed exercise therapy should follow in order to achieve an optimal result.
Similar to the technique of neurectomy, selective myotomy and also myectomy is intended to achieve a targeted elimination of muscle subgroups. While myotomy involves the targeted severing of the hyperactive muscle, myectomy aims at the complete removal of the muscle. In the case of severed but unremoved muscles, the function can be restored by the merging of the cut edges.[1]
The techniques of neurectomy and myotomy/myectomy both aim at significantly improving the symmetry of the face halves. In particular after a successful gracilis muscle transfer (here please link to free muscle transplants), the patient's attention seems to shift from the resanimation of the smile to the improvement of asymmetry, especially in the region of the lower lip.[2] Basically, muscle subgroups are addressed which can be dispensed with in favor of functionally much more important antagonists. If, for example, the muscles that often lower the corner of the mouth in patients with facial nerve palsy are specifically weakened or eliminated, this leads to easier lifting of the corner of the mouth and upper lip.[3] Interestingly, a myectomy/myotomy of the muscles that lower the corner of the mouth (here please link to Muscles of Facial Expression) can lead to an improved emotional expression of anger and sadness, although it is precisely this muscle group that is responsible for an upset or sad facial expression.[4] A publication by Edgerton in 1966 had for years suggested that removal of the lower lip depressor (M. depressor labii inferioris) could cause speech deficits. Recent scientific studies revise this conclusion and even assume an improvement in speech postoperatively. Furthermore, all three methods represent therapeutic options for the treatment of synkinesis (here please link to Synkinesis).[5,6]
This young patient showed the typical symptoms of synkinesia and dyskinesia after defective healing of Bell's paresis. He received a selective neurectomy, a muscle transfer in the mouth area and a partial removal (myectomy) of the platysma muscle in one procedure. After the operation, the face is more balanced with significantly less spastic hyperactivity. The left corner of the mouth is considerably freer, the negative vector during smiling (corner of the mouth facing down) has disappeared. The function of the muscles that lift the upper lip is also improved: before the operation, only 1.5 upper teeth were visible in broad laughter; after the operation, 3.5 upper teeth and a clearly straight lip are now visible.
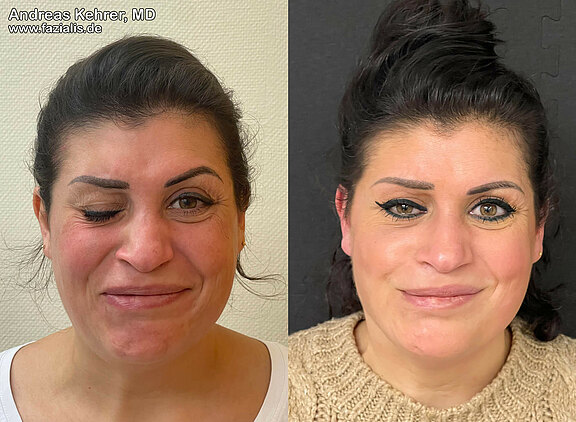
This 35-year-old female patient suffered from severe synkinesia after defect healing of the facial nerve in the right side of her face. She complained of uncontrollable eye closure when smiling, marked and sometimes painful spasms of the midface, mouth region, and neck. Analysis revealed uncoordinated muscle activity at the corner of the mouth. A so-called negative vector (corner of the mouth on the right side points downwards despite smiling) can be seen. After a targeted removal of several nerve branches (selctive neurolysis, selective neurectomy) and a muscle transposition as well as partial removal (all in one operation) via a facelift incision, the face appears much more balanced. The lady is able to smile more symmetrically, the eye remains open, the painful muscle tensions have been further relieved, and the annoying retractions in the chin area have also been reduced. Consistent exercise therapy is now indicated to further improve the surgical result. The patient's quality of life has already improved massively.
Sources:
[01] Vincent, A. G., Bevans, S. E., Robitschek, J. M., Wind, G. G., & Hohman, M. H. Masseteric-to-Facial Nerve Transfer and Selective Neurectomy for Rehabilitation of the Synkinetic Smile. JAMA Facial Plastic Surgery 2019. doi:10.1001/jamafacial.2019.0689.
[02] vanVeen MM,Dusseldorp JR,Hadlock TA. Long-term outcome of selective neurectomy for refractory periocular synkinesis. Laryngoscope. 2018;128(10):2291-2295. doi:10.1002/lary.27225.
[03] Azizzadeh, B., & Frisenda, J. L. Surgical Management of Postparalysis Facial Palsy and Synkinesis. Otolaryngologic Clinics of North America 2018. doi:10.1016/j.otc.2018.07.012.
[04] Hjelm N, Azizzadeh B. Modified Selective Neurectomy with Symmetrical Facial Repositioning. Facial Plast Surg Aesthet Med. 2020;22(1):57-60. doi:10.1089/fpsam.2019.29005.hje.
[05] Hussain G, Manktelow RT, Tomat LR. Depressor labii inferioris resection: an effective treatment for marginal mandibular nerve paralysis. Br J Plast Surg. 2004 Sep;57(6):502-10. doi: 10.1016/j.bjps.2004.04.003. PMID: 15308395.
[06] Lindsay RW, Edwards C, Smitson C, Cheney ML, Hadlock TA. A systematic algorithm for the management of lower lip asymmetry. Am J Otolaryngol. 2011 Jan-Feb;32(1):1-7. doi: 10.1016/j.amjoto.2009.08.011. Epub 2009 Oct 9. PMID: 20015805.
[07] Chen CK, Tang YB. Myectomy and botulinum toxin for paralysis of the marginal mandibular branch of the facial nerve: a series of 76 cases. Plast Reconstr Surg. 2007 Dec;120(7):1859-64. doi: 10.1097/01.prs.0000287136.22709.77. PMID: 18090747.
[08] Hussain G, Manktelow RT, Tomat LR. Depressor labii inferioris resection: an effective treatment for marginal mandibular nerve paralysis. Br J Plast Surg. 2004 Sep;57(6):502-10. doi: 10.1016/j.bjps.2004.04.003. PMID: 15308395.
[09] Chuang DC, Chang TN, Lu JC. Postparalysis facial synkinesis: clinical classification and surgical strategies. Plast Reconstr Surg Glob Open. 2015 Apr 7;3(3):e320. doi: 10.1097/GOX.0000000000000283. PMID: 25878931; PMCID: PMC4387142
[10] Azizzadeh B, Irvine LE, Diels J, Slattery WH, Massry GG, Larian B, Riedler KL, Peng GL. Modified Selective Neurectomy for the Treatment of Post-Facial Paralysis Synkinesis. Plast Reconstr Surg. 2019 May;143(5):1483-1496. doi: 10.1097/PRS.0000000000005590. PMID: 30807497.