Contrary to the widely used term "paresis", which is used synonymously in clinical everyday life as a term for paralysis, strictly speaking a difference is made between the different types. Paresis describes a partial malfunction of one or more muscle groups with incomplete paralysis. In contrast, complete paralysis of individual muscles or entire muscle groups is referred to as paralysis (in any type of musculature, including intestinal muscles) or plegy (only in skeletal muscles) [1,2].
The symptoms of paralysis of the facial nerve have been known for centuries. Documentation dates back to 1797, when the German professor Nicolaus Anton Friedreich recorded the successful treatment of three patients with paralysis of the facial nerve [3]. About a quarter of a century later, Sir Charles Bell wrote a detailed treatise on idiopathic facial nerve palsy (IFNP), which was later named after him as "Bell´s palsy" or "Facial nerve palsy after Bell" [4].
In general, a distinction is made between a central or peripheral type of paralysis and an irreversible and spontaneously receding paresis. The Gyrus praecentralis (primary motor cerebral cortex, cell body of the first motor neuron), as the most important origin of the so-called pyramidal tract, sends afferences to the two cell groups of the ncl. n. facialis (cell body of the second motor neuron) via the fibrae corticonucleares (part of the pyramidal tract).
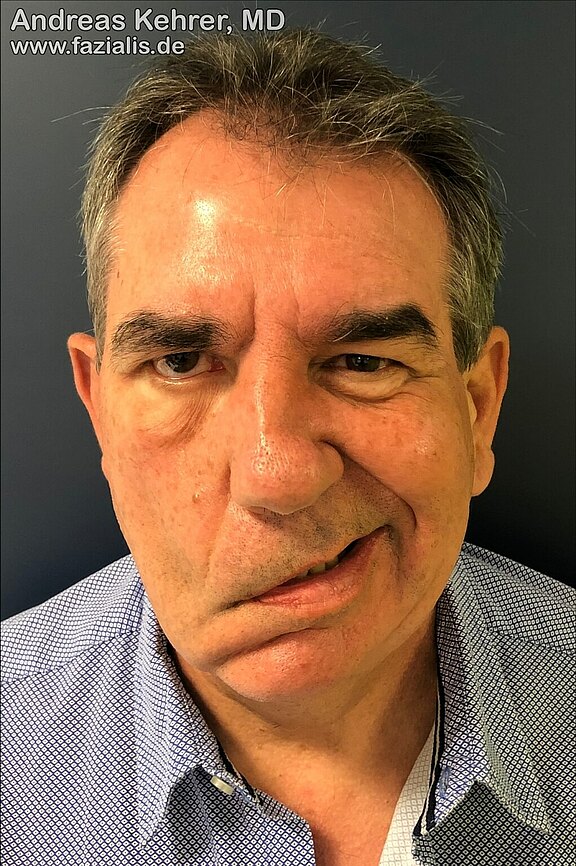
The upper cell group supplies the eyelid and forehead muscles and is controlled by the ipsilateral as well as the contralateral pre-central region (on both sides). The lower nuclear cell group, which is responsible for the innervation of the remaining mimic muscles, is only controlled by crossed fibers of the contralateral side. Thus, the differentiation between a central and a peripheral paralysis of the facial nerve allows conclusions to be drawn about the location of the lesion with respect to the facial nerve [4,5]:
| central facial paresis | peripheral facial paresis |
|---|---|
| Damage in front of the brain nuclei of the facial nerve | lesion beneath the brain nuclei of the facial nerve |
| intact forehead muscles on both sides and | Paralysis depends on the lesion site: |
| paralyzed residual mimic musculature | Paresis of individual muscles up to the entire |
| on the opposite side of the face | mimic musculature of the same facial side |
You can learn more about the interconnection of the facial nerve cores in the brain here. Further information on electrophysiological diagnostics by a neurologist can be found here.
Sources:
[1] Aumüller G. Anatomie. 3rd ed. Duale Reihe. Stuttgart: Thieme; 2014. 54 p. ger
[2] Masuhr KF, Masuhr F, Neumann M. Neurologie. 7th ed. Duale Reihe. ger.
[3] Bird TD. Nicolaus A. Friedreich's description of peripheral facial nerve paralysis in 1798. J Neurol Neurosurg Psychiatry. 1979;42(1):56–8. PubMed PMID: 368292.
[4] Bell C. On the Nerves; Giving an Account of Some Experiments on Their Structure and Functions, Which Lead to a New Arrangement of the System. Philosophical Transactions of the Royal Society of London. 1821;111(0):398–424. doi: 10.1098/rstl.1821.0029.
[5] Schünke M, Schulte E, Schumacher U, Voll M. Kopf, Hals und Neuroanatomie: 115 Tabellen. 2nd ed. Prometheus / Michael Schünke Erik Schulte Udo Schumacher. Unter Mitarb. von Jürgen Rude. Ill. von Markus Voll Karl Wesker, Vol 3. Stuttgart: Thieme; 2009. 541 p. ger.
[6] Peitersen E. Bell's palsy: the spontaneous course of 2,500 peripheral facial nerve palsies of different etiologies. Acta Otolaryngol Suppl. 2002(549):4–30. PubMed PMID: 12482166.