Psyche and mental health of patients with facial palsy: affected patients suffer greatly from reduced function of the facial nerve, which results in severe functional and aesthetic impairments. The facial nerve has the unique ability to be the only nerve that enables an individual to respond "emotionally" to his or her environment. Among the many other forms of facial expression, smiles and laughter play a critical role in social interaction.
If facial nerve function is disturbed, a disfiguring "facial nerve palsy" often results. The result is an uncontrolled "derailment of facial features". On the psychosocial level, this can cause severe difficulties in communication. Due to the stigmatizing asymmetry, affected patients unfortunately often show a reduction in self-esteem and a conscious restraint of emotions towards the environment. This phenomenon can be observed because consciously controlled facial expressions increase the asymmetry. Often a concrete avoidance behavior of the patients in society can also be observed, with concentration of social activities on family and close friends. Of course, this does not have to apply to every individual, but these behavioral patterns frequently occur.
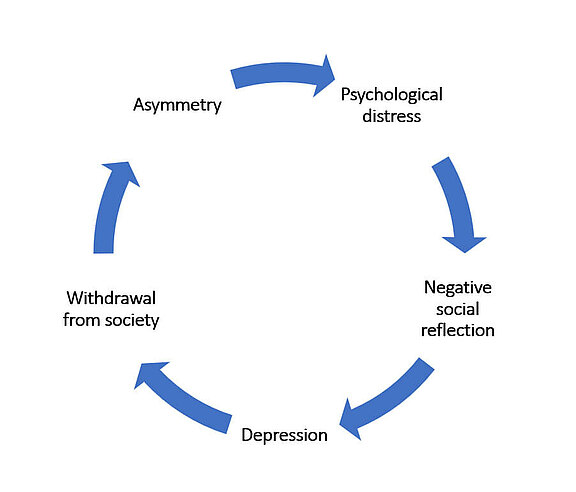
Figure 1
Asymmetry and significant restrictions of the remaining facial expressions affect the patients in their social interaction. The partly negative emotional (mimetic) resonance of fellow human beings intensifies tendencies to withdraw from society and reduces self-esteem. The prevalence of depression in patients with facial paralysis is 5 times higher than in the normal population.
A study by Aaron Kosins et al. at the Facial Palsy Clinic in Edinburgh, Scotland, showed that in a collective of 22,954 patients with facial nerve paresis over 50% display considerable psychological stress and concrete withdrawal tendencies from society[1]. Persons with facial paralysis have a 65% prevalence of depression, five times the unaffected population[2]. Dealing with social contacts and reactions of the environment is particularly difficult for these patients[3].
At the beginning, displacement mechanisms appear to be sufficient. In the further course, so much mental and physical energy is demanded from the patient to master daily life, deal with the disease, and with other people resulting in psychological and physiological symptoms fatigue. The compensation of these is no longer possible and the psychological suffering increasingly manifests itself clinically[3]. Huang et al (2012) were able to establish a clear connection between psychological stress and the severity of facial paralysis[4].
Patients stigmatized by facial paralysis often retreat into themselves which leads to social rejection. In addition to disturbed non-verbal communication, they also restrict verbal communication. The patients avoid any facial expressions that could still emphasize the stigma; quite a few even turn away from the interlocutor or try to hide the disturbed parts of the face behind their hands[5].Unfortunately, this often leads to a false picture of the person's personality, as the limited facial expression is misinterpreted as coldness of feeling, lack of interest, or passivity[5,6]. Dobel et al. (2013) also described interpersonal communication disorders in facial palsy patients. The patients complained mainly that the sight of their face caused negative feelings in fellow human beings and that their inner emotional state could
Dysfunction in the region of the mouth is said to have the greatest influence on the emotional milieu of patients. In a study by Neely and Neufeld, patients felt facial paralysis worse than synkinesis in the area of the mouth, while synkinesis was experienced as the more debilitating limitation in the area of the eye complex[6]. At the beginning of the facial paralysis, the functional restriction the eye is the most concerning region, while later the perioral region dominates; the greatest wish of many patients is a beautiful, "normal" smile[8]. By restricting the smile, the patient experiences less positive reactions. Additionally, there are empirical results which demonstrate that the activation of the zygomaticus major muscle and peripheral feedback from the smile contribute to positive emotions[2].
Facial neuromotor disorders do not show a greater general impairment of facial movements in patients with depression, but a greater impairment of the smile compared to the non-depressed patients[2]. Pensak et al. postulate that patients are more affected by psychological restrictions than by physical symptoms. This is confirmed by Van Swearingen et al., who found that physical, social, and emotional difficulties at the individual level correlated more strongly with anxiety and depression, than physical and anatomical problems at the organ or tissue level. In the development of social problems based on neuromuscular disorder after facial paralysis, not enough attention is paid to its psychological ramifications[3].
A patient from our cohort described for us her emotional world in connection with her facial paralysis particularly aesthetically:
"At the young age of 36, I was struck by a bolt of lightning out of the blue, suddenly 40 years old, looking and feeling like an unfortunate stroke patient! Nobody could really help me. This plunged me into a deep crisis and depression that I had to struggle with for years..."
You can read the detailed description and how the story ended positively for the lady here.
Resting symmetry of the face is often very well preserved in young patients. The missing facial expression of the paralyzed side is typically concealed by a general omission of facial expressions. This is also the case with this 23-year-old patient. When asked to demonstrate a full, broad smile, he only reveals a suggestive, barely perceptible smile. Just as much movement as the paralyzed side allows. He has virtually "forgotten" a more intensive facial expression through his paralysis. The consciously limited facial expression can easily be misinterpreted by the environment.
Sources:
[1] Kosins AM, Hurvitz KA, Evans GR, Wirth GA. Facial paralysis for the plastic surgeon. Can J Plast Surg. 2007;15(2):77–82. PubMed PMID: 19554190.
[2] Van Swearingen JM, Cohn JF, Bajaj-Luthra A (1999) Specific Impairment of Smiling Increases the Severity of Depressive Symptoms in Patients with Faicial Neuromuscular Disorders. Aesth Plast Surg 23: 416-423
[3] Van Swearingen JM, Cohn JF, Turnbull J, Mrzai T, Johnson P (1998) Psychological distress: Linking impairment with disability in facial neuromotor disorders. Otolaryngol Head Neck Surg 118: 790-796
[4] Huang B1, Xu S, Xiong J, Huang G, Zhang M, Wang W. Psychological factors are closely associated with the Bell's palsy: a case-control study. J Huazhong Univ Sci Technolog Med Sci. 2012 Apr;32(2):272-9
[5] Kiese-Himmel C, Laskawi R, Wrede S (1993) Psychosocial Problems and Disease Processing of Patients with Defect Healing after Facialis Paresis. 41: 261-267
[6] Neely JG, Neufeld PS (1996) Defining Functional Limitation, Disability, and Societal Limitations in Patients with Facial Paresis: Initial Pilot Questionnaire. Am J Otol 17: 340-342
[7] Emotional Impact of Facial Palsy - C. Dobel et. al, Laryngo-Rhino-Otol 2013; 92: 9–23
[8] Faulty regeneration of the facial nerve - a neglected clinical picture - Wolowski A, Inaugural dissertation 2005, University Hospital Münster