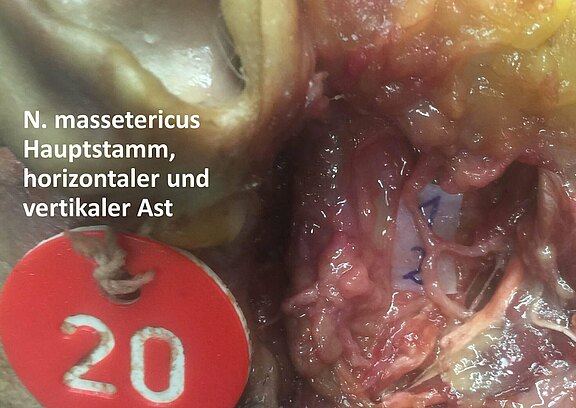
We have been conducting extensive basic research into the nervous system of the face on anatomical specimens of body donors based on scientific studies for years. The aim of these studies is to improve surgical methods and clinical applications. In one of the largest series of studies worldwide, the macro- and microanatomy and other important basics of the facial nerve and other donor nerves important for the plastic reconstruction, such as the masticatory nerve (masseteric nerve), could be examined in detail on more than 100 facial halves. As a consistent goal, a comprehensive representation of the axon capacities (number of nerve fibers) of the entire facial nerve branch system in the face was formulated at clinically relevant sections for facial reanimation (reanimation of facial expressions, i.e. potential connection points for nerve transplants and functional muscle transplants). Another relevant donor nerve branch for neurotizing procedures should be the masseteric nerve (Radix motoria nervi trigemini). This objective should be based on a high number of preparations, since in the current international literature feature only very few corresponding studies with a higher number of samples were found. For this purpose, the branches of the facial nerve and the masseteric nerve were prepared in this study using 53 body donors (fresh frozen) and a total of 106 facial halves under four times magnification. A detailed photo documentation and description of the anatomical connections (number of main and lower branches, diameters, fusions, nerve anastomoses and lower crossings) was carried out in parallel.
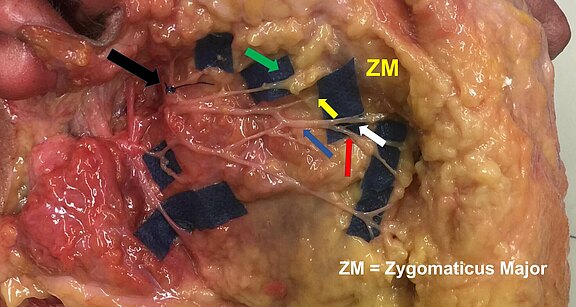
The author of this page and his team have microsurgically dissected and scientifically examined more than 100 facial halves of "fresh-frozen" human body donors. The complex nerve plexus in the area of the zygomatic and buccal branch systems, which is essentially important for facial nerve reconstruction, was a focal point of the research work.
This 3D model impressively demonstrates the complicated anatomy of the face. Detailed anatomical knowledge is indispensable (conditio sine qua non) for successful and safe surgical results. The complex arrangement of the mimic musculature in several planes, the sensitive, motor and autonomous nervous systems, the arteries and veins, salivary glands and other structures are clearly visible. Intensive in-house research work has made a significant contribution to a better understanding of the anatomic relations of facial structures.
Source: "aherrler". Half of a head without skin. 2019. sketchfab.com/3d-models/half-of-a-head-without-skin-515c6f9c71784996bfab4fdb80ef0ad9 . Accessed on 11/15/2020. CC BY-SA 4.0. creativecommons.org/licenses/by-sa/4.0.
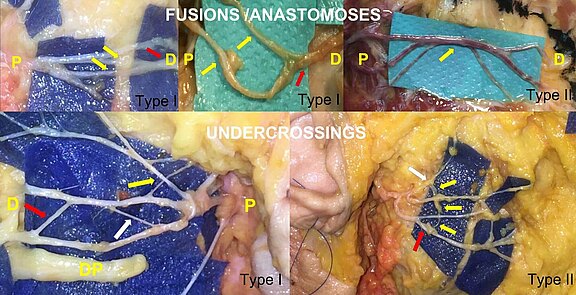
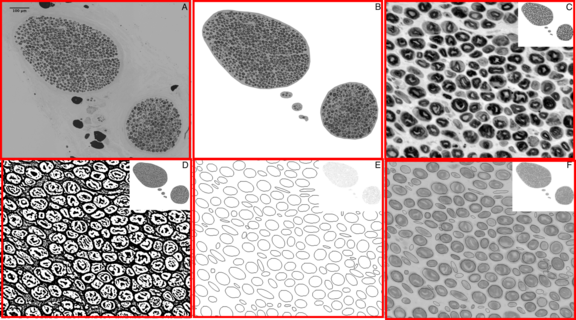
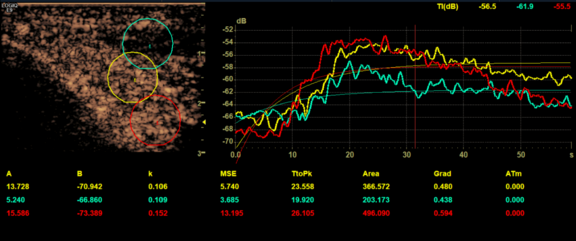
About 1200 nerve samples were taken to investigate the number of nerve fibers (axons), fascicle structure, axon density, microscopic diameter determination, and other details of various nerve branches. The nerve fiber capacity sometimes determines how strongly the musculature is addressed for facial expression. The facial nerve shows a highly variable branching pattern with large individual differences between different patients and even the halves of the face within a face. Contrary to the previously known studies, the facial nerve could for the first time be described in a three-dimensional pattern instead of in a two-dimensional form (in one plane) and the exchange of fibers between individual nerve branches could be investigated more closely. In addition, new forms of lower crossings of nerve branches were discovered which showed no fiber exchange.
After fixation and preparation of semi-thin sections, the preparations were stained with a Richardson staining solution and PPD staining (paraphenylenediamine for nerve staining of osmated semi-thin sections). The histological sections were then digitized. This enabled semi-automated computer-based counting of myelinated axons.
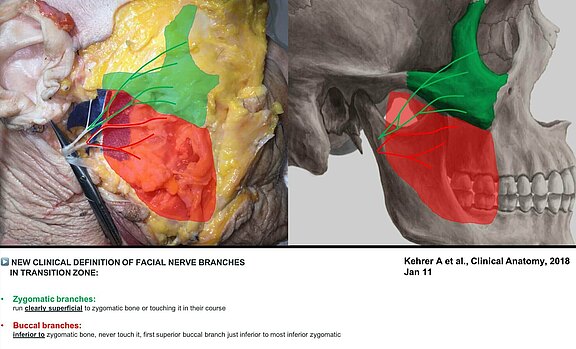
A main focus of our research work is also the exact description of the nerve supply of an important muscle called "Zygomaticus major". It is the main actor of the lateral lifting of the corner of the mouth, the strongest laugh/smiling muscle, and thus one of the most important muscles for facial expression. Our research team was able to define a new anatomical definition for the precise description of its nerve supply in relation to surrounding anatomical structures.
Based on our gained macroanatomical knowledge, a new clinically-oriented definition was formulated for the precise differentiation of the zygomatic and buccal branches of the facial nerve in the zygomatico-buccal system in the context of facial reanimation. In 96 investigated facial halves, zygomatic branches innervated the relevant Zygomaticus major muscle in 64 cases (67%, 95% CI: 56% to 76%). Buccal nerve branches innervated it in 32 facial halves (33%, 95% CI: 24% to 44%). No significant differences in sex or lateral orientation were found. Significant differences of nerval control between men and women and also the right and left half of the face were not found. A self-developed, computer-assisted procedure was also used to precisely determine the nerve fiber capacities of the facial nerve.
The diameter of the nerve branch, the location of the donor nerve, and the nerve fiber capacity are among other things critical for the success of a free functional muscle transplant to give the paralyzed face the desired muscle tension (tonus) and mobility (muscle contractility) again. The scientific results from our research laboratory have already been transferred directly into clinical practice and have significantly improved the functional results for patients in terms of facial expression, symmetry, aesthetics, and facial tone.
In one of our microanatomical studies, the axon capacity of the extratemporal facial nerve main trunk was measured using computer-based semi-automatic quantification. Furthermore, the fascicular structure was assessed and the main trunk diameter measured. 3.82 fascicles (1-9 fascicles) were found in the main trunk (n=97). An average axonal capacity of 6684 ± 1884 axons (range: 2655 to 12457) was determined on 87 halves of the face. Right facial hemispheres showed 6364 ± 1904 axons (n=43), left 6996 ± 1833 axons (n=44) with a p=0.73. Female preparations showed 6247 ± 2230 (n=22), male 6769 ± 1809 nerve fibers (n=40) without statistical difference (p=0.59). The nerve diameter was measured with 1933 ± 424 µm (975 - 3012) (n=82). Possible potential donor nerves for neurotization including their specific axon capacities are discussed in the publication in connection with the results found.
As a donor nerve for neurotizing procedures, but also for free functional muscle transplantation, we often use the masseteric nerve - a branch of the masticatory muscle nerve. Due to its topographical proximity to the main trunk of the facial nerve and the zygomatic and buccal branch systems, neurotizing operations (nerve transfers) with only one coaptation (nerve suture) can be performed instead of two coaptations required in older procedures such as the hypoglossus jump nerve anastomosis. The nerve to the masseter is a strong donor with minimal loss of axon capacity (high degree of motor input to target).
Furthermore, contrary to the technique with a hypoglossus jump nerve anastomosis, the removal of an additional donor nerve (such as the auricularis magnus nerve) is not necessary when using the masseteric nerve and avoidable sensitivity disorders (e.g. numb outer ear after removal of the donor nerve) do not occur. An impairment of the chewing function is not to be expected. Synkinesis can also be expected when using the masseteric nerve. However, there are indications in the literature that these are less significant than with other donor nerves.
The representation of the smallest vessels plays an important role in microsurgery. It makes it considerably easier for the microsurgeon to plan even the most complex reconstructions safely before surgery. According to the author, it should be performed directly by the surgeon in order to achieve the greatest possible safety for the patient on the one hand and the shortest possible operation time on the other. The author has therefore conducted a study on head and neck patients in Taiwan as part of one of his fellowships (further specialization) in order to investigate the accuracy of the so-called color-coded duplex ultrasound for its suitability for the design of flap plasty of the thigh for complex reconstructions. For this purpose, he examined the corresponding patients immediately before the operation on the operating table according to a standardized protocol and compared the actual anatomical conditions of the smallest perforator vessels important for flap design during the subsequent flap reconstruction. For example, all the vessels visualized in ultrasound were also found during the subsequent microsurgical operation. The precision of the ultrasound diagnostics was so high that the average of the targeted perforator vessel was only slightly more than 2 mm away from the actual anatomical localization. The study was published in a prestigious international journal for microsurgery [4].
Sources:
[1] Kehrer A, Mandlik V, Taeger C, et al. Postoperative control of functional muscle flaps for facial palsy reconstruction: ultrasound guided tissue monitoring using contrast enhanced ultrasound (CEUS) and ultrasound elastography. Clin Hemorheol Microcirc 2017
[2] Kehrer A, Engelmann S, Bauer R, et al. The nerve supply of zygomaticus major: Variability and distinguishing zygomatic from buccal facial nerve branches. Clin Anat 2018
[3] Kehrer A, Engelmann S, Bauer R, Geis S, Kehrer M, Prantl L, Bleys RLAW, Mandlik V. Anatomical study of the zygomatic and buccal branches of the facial nerve: application to facial reanimation procedures. Clin Anatom 2019
[4] Kehrer A, Engelmann S, Ruewe M, Geis S, Taeger C, Kehrer M, Tamm ER, Bleys RLAW, Prantl L, Mandlik V. Perfusion maintains functional potential of denervated mimic muscles in early persistent facial paralysis which requires early microsurgical treatment - the histoanatomic basis of the extratemporal facial nerve trunk assessing axonal load in the context of possible nerve transfers. Clin Hemorheol Microcirc. 2018
[5] Mandlik V, Ruewe M, Engelmann S, Kehrer A. Significance of the Marginal Mandibular Branch in Relation to Facial Palsy Reconstruction - Assessment of Micro- and Macroanatomy including Axonal Load in 96 Facial Halves. Annals of Plastic Surgery 2019
[6] Engelmann S, Ruewe M, Geis S, Taeger CD, Kehrer M, Tamm ER, Bleys RLAW, Zeman F, Prantl L, Kehrer A. Rapid and Precise Semi-Automatic Axon Quantification in Human Peripheral Nerves. Sci Rep. 2020
[7] Sommerauer L, Engelmann S, Ruewe M, Anker A, Prantl L, Kehrer A. Effects of electrostimulation therapy in facial nerve palsy. Arch Plast Surg. 2020
[8] Ruewe M, Engelmann S, Huang CW, Klein SM, Anker AM, Lamby P, Bleys RLAW, Tamm ER, Prantl L, Kehrer A. Microanatomy of the Frontal Branch of the Facial Nerve: The Role of Nerve Caliber and Axonal Capacity. Plast Reconstr Surg. 2021
[9] Kehrer A, Ruewe M, Platz Batista da Silva N, Lonic D, Heidekrueger PI, Knoedler S, Jung EM, Prantl L, Knoedler L. Using High-Resolution Ultrasound to Assess Post-Facial Paralysis Synkinesis-Machine Settings and Technical Aspects for Facial Surgeons. Diagnostics (Basel). 2022
[10] Knoedler L, Baecher H, Kauke-Navarro M, Prantl L, Machens HG, Scheuermann P, Palm C, Baumann R, Kehrer A, Panayi AC, Knoedler S. Towards a Reliable and Rapid Automated Grading System in Facial Palsy Patients: Facial Palsy Surgery Meets Computer Science. J Clin Med. 2022
[11] Knoedler L, Miragall M, Kauke-Navarro M, Obed D, Bauer M, Tißler P, Prantl L, Machens HG, Broer PN, Baecher H, Panayi AC, Knoedler S, Kehrer A. A Ready-to-Use Grading Tool for Facial Palsy Examiners-Automated Grading System in Facial Palsy Patients Made Easy. J Pers Med. 2022
[12 ] Kehrer A, Ruewe M, Klebuc M, Platz Batista da Silva N, Lonic D, Heidkrueger P, Jung EM, Prantl L, Knoedler L. Objectifying the Role of the Depressor Anguli Oris Muscle in Synkinetic Smile Formation with High-Resolution Ultrasound- A Prospective Study. Plastic Recon Surg 2023
[13 ] Knoedler, L; Knoedler, S; Chartier, C; Panayi, A.; Orgill, D; Moog, P; Oezdemir, B; von Isenburg, S; Studier-Fischer, A; Prantl, L; Kehrer, A..The Rise of Facial Palsy on Social Media Over the Last 5 Years. Journal of Craniofacial Surgery 2022
[14 ] Kehrer A, Hollmann KS, Klein SM, Anker AM, Tamm ER, Prantl L, Engelmann S, Knoedler S, Knoedler L, Ruewe M. Histomorphometry of the Sural Nerve for Use as a CFNG in Facial Reanimation Procedures. J Clin Med. 2023
[15] Knoedler S, Knoedler L, Hoch CC, Kauke-Navarro M, Kehrer A, Friedman L, Prantl L, Machens HG, Orgill DP, Panayi AC. An ACS-NSQIP Data Analysis of 30-Day Outcomes Following Surgery for Bell's Palsy. J Craniofac Surg. 2023
[16] Kehrer A, Engelmann S, Knoedler L, Klein S, Anker A, Heidekrueger P, Tamm E, Bleys R, Prantl L, Ruewe M. The masseteric nerve for facial reanimation: Macroscopic and histomorphometric characteristics in 106 human cadavers and comparison of axonal ratio with recipient nerves. Journal of Cranio-Maxillofacial Surgery 2023
[17] Knoedler L, Alfertshofer M, Simon S, Prantl L, Kehrer A, Hoch CC, Knoedler S, Lamby P. Diagnosing lagophthalmos using artificial intelligence. Sci Rep. 2023